Gastric cancer ranks among the most widespread diseases in Asian populations, with South Koreans experiencing the third-highest incidence globally in 2020, as reported by the International Agency for Research on Cancer. Recently, a collaborative research effort between Pohang University of Science and Technology (POSTECH) and Yonsei University achieved advancement in the realm of precision personalized medicine for gastric cancer. By using 3D bioprinting to accurately replicate the biological environment surrounding gastric cancer cells, the researchers have achieved a significant feat—predicting a patient’s response to anticancer drugs during the preclinical stage. This marks a significant milestone in the exploration of precision personalized medicine for gastric cancer.

Clinical trials, aimed at assessing the efficacy of new drugs or treatments, are typically conducted on humans. The ability to predict patient responses during the preclinical phase is crucial for selecting suitable candidates for these trials. This not only helps in minimizing unexpected side effects but also enhances the overall success rates. Unfortunately, existing technologies face limitations in accurately replicating the pathology of gastric cancer and the intricate environment surrounding the tumor in vitro.
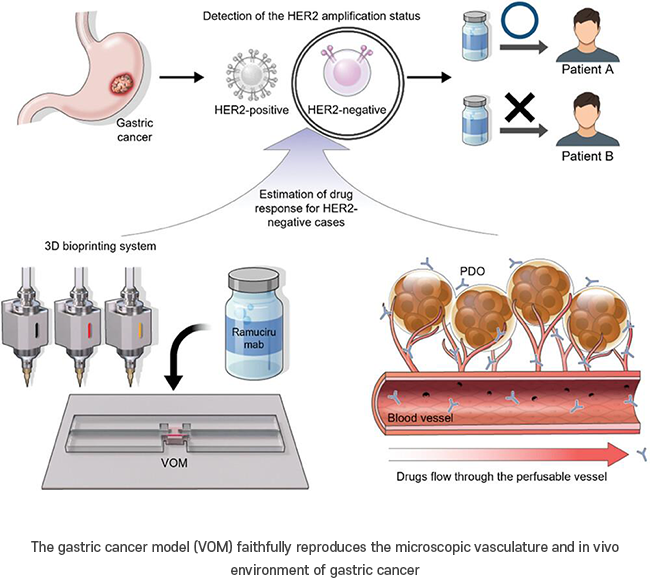
To address this challenge, the research team used organoids obtained from gastric cancer patients along with 3D bioprinting technology. This approach led to the development of a vascularized organoid model (VOM)*2 that faithfully reproduces the actual vasculature and environment of gastric cancer. The incorporation of a stomach-derived decellularized extracellular matrix (st-dECM)*3, rich in stomach-specific matrix proteins such as collagen, contributed to a high cell viability rate exceeding 90%. Furthermore, the model demonstrated a high level of similarity to actual gastric cancer conditions.
Based on these findings, the team generated patient-specific vascularized organoid models (VOMs) for use in drug trials. The outcomes revealed distinct responses to the same drug among different patient models, aligning with real-world clinical trial results. The created VOMs, faithfully replicating the microscopic vasculature and biological conditions of gastric cancer, enabled the team to predict patient responses during the preclinical stage.
Furthermore, the VOM accurately mimicked the clinical response to the vascular endothelial growth factor receptor (VEGFR2). The research highlighted the limitation of the currently employed human epithelial cell proliferation factor receptor (HER2) as the sole target in clinics, underscoring its ineffectiveness for patients unresponsive to this target. This research creates new possibilities for a broader spectrum of therapies.
Professor Jinah Jang who led the research stated, “We have developed a promising platform for personalized cancer treatment.” She added, “This platform has potential applications in other types of cancer where drugs act through the blood vessels.” Professor Jae-Ho Cheong from Yonsei University remarked, “The advanced biomodel platform is crucial in simulating diverse clinical trials at the laboratory level. It not only facilitates the study of cancer mechanisms but also enables the advance assessment of the effectiveness of anticancer drugs, offering a new paradigm for the implementation of precision medicine in cancer.”

This research was supported by Korean Fund for Regenerative Medicine funded by Ministry of Science and ICT, and Ministry of Health and Welfare, the Korea Institute for Advancement of Technology (KIAT) and the Ministry of Trade, Industry & Energy(MOTIE) of the Republic of Korea, and National Cancer Center. This study was partly supported by the National Research Foundation of South Korea (NRF) grant funded by the Ministry of Science and ICT and the Korean government (MSIP), and Basic Science Research Program through the National Research Foundation of Korea(NRF) funded by the Ministry of Education.