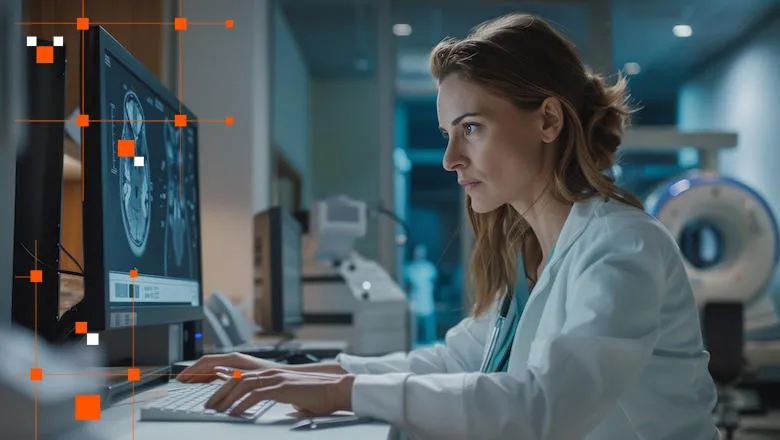
The key challenge highlighted in the study is the need for quick and accurate identification of COVID-19 cases to control the spread of the virus effectively. Whilst the accepted best diagnostic test for COVID-19 (called reverse transcriptase polymerase chain reaction or RT-PCR)) should not be omitted or replaced, it does take hours to process. Therefore, researchers explored the use of CT angiography (CTA) imaging, a technique commonly used to assess suspected acute stroke patients, as a tool to detect COVID-19-related lung abnormalities.
A specific type of lung abnormality called ground-glass opacity (GGO), visible on CTA scans of the lung apices, emerged as a potential identifier for COVID-19.
The COVID-SALES 2 study is the follow-up to the landmark first COVID-SALES study (published in 2020). Undertaken in collaboration with the Radiology Academic Network for Trainees (RADIANT), this prospective multicentre study expanded on the scope of the first study, with data collected from 13 UK hyperacute stroke units. The findings have reinforced the clinical utility of lung apical changes on routine CT angiography studies in the incidental diagnosis of COVID-19.
Jason Mak, Clinical Radiology SpR, RADIANT Co-chair
In summary, we recommend routinely analysing lung apices in patients with stroke undergoing carotid CTA, because this rapid and easy assessment of apices is valuable, opportunistic, and “free” information in a routine and unmodified scan. The apical analysis simply identifies patients likely to have COVID-19 with early downstream benefits such as limiting disease transmission.
Dr Thomas Booth, Reader in Neuroimaging, School of Biomedical Engineering & Imaging Sciences
Previous research in London hospitals during the first year of the pandemic by the same team has already suggested that GGO could be a reliable indicator of COVID-19 infection and prognosis. To validate this finding in all patients with acute stroke, it was important to test it on patients from hospitals throughout an entire nation with prospective data collection at a subsequent time point in the pandemic. The study, following strict guidelines for diagnostic accuracy research, enrolled over a thousand patients from thirteen healthcare sites. Among these patients, approximately 8.5% exhibited apical GGO, and further testing revealed that 5.1% of them were positive for COVID-19.
The absence of scanned GGO also showed a high negative predictive value (99.7% in vaccinated patients), meaning it accurately ruled out COVID-19 in most cases. This indicates that GGO could serve as a valuable tool for quickly excluding COVID-19, especially in patients presenting with symptoms of stroke.
Alongside validating the reliability of GGO as a COVID-19 identifier, the study also emphasises its ease of interpretation, even among less experienced radiologists. “This suggests that firstly, radiologists (and other healthcare professionals) should actively review the lung apices on CTA in all stroke patients and comment on GGO presence or absence, and secondly, that incorporating CTA imaging into COVID-19 triage protocols in stroke patients could streamline the process and improve patient management.
“In our hospitals, apical analysis is now articulated in reports to good effect, for example, changing staff personal protective equipment requirements (e.g., from a fluid-repellant surgical mask to an FFP3 or N95 mask), and directing a patient to a side room instead of an open ward, pending RT-PCR results”, said Dr Booth.
This research underscores the importance of leveraging imaging techniques like CTA to enhance COVID-19 triage efforts, particularly in high-pressure environments like emergency departments.