Researchers at the University of Toronto and its partner hospitals have created a unique heart-on-a-chip model that is helping untangle the causes of COVID-19-induced heart inflammation and uncover strategies to reduce its impact.
While COVID-19 is primarily a respiratory infection, clinicians and researchers are increasingly aware of the virus’s effects on other organs – including the heart. Data from the U.S. Centers for Disease Control and Prevention shows patients hospitalized with COVID-19 between March 2020 and January 2021 had 15 times higher risk for developing myocarditis, or inflammation of the heart muscle, compared to patients without COVID-19.
But the biology behind the association between SARS-CoV-2 infection and heart inflammation had remained unclear – in part because there have not been good models with which to study infection-related heart inflammation.
“Conventionally, people grow heart cells in a 2D setting and then expose it to SARS-CoV-2 to see how the virus damages the heart. But that’s not actually what happens in our body,” says Rick Lu, a PhD graduate from U of T’s Institute for Biomedical Engineering who is currently a postdoctoral researcher at U of T’s Leslie Dan Faculty of Pharmacy.
Lu is the first author of a new study that describes a miniature 3D heart-on-a-chip model that more accurately captures the impact of SARS-CoV-2 infection and its associated immune response on cardiac dysfunction.
The first-of-its-kind model builds on previous work led by Milica Radisic, Lu’s PhD adviser, a senior scientist at University Health Network and a U of T professor of biomedical engineering. The approach uses a lab-made network of blood vessels surrounded by heart tissues grown from stem cells to mimic a real human heart with its tangle of vessels going in and out.
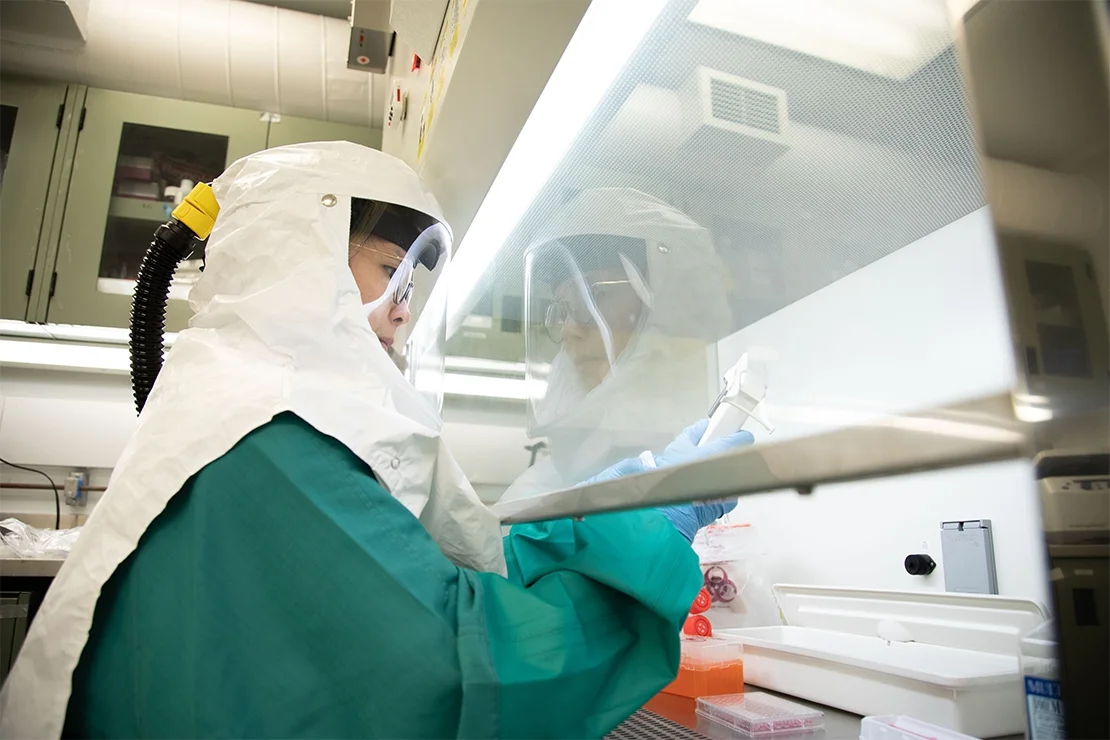
To examine the effects of COVID-19 on heart inflammation, Lu and his colleagues first had to adapt their model to work in the , a specialized lab that allows researchers to study high-risk pathogens like SARS-CoV-2 in a safe and secure way.
“This work would simply not be possible without the Toronto High Containment Facility,” says Radisic, who holds the Canada Research Chair in Organ-on-a-Chip Engineering.
In the high containment lab, the researchers added live virus and immune cells to the blood vessels and allowed them to flow through their mini hearts-on-a-chip, replicating the immune response that happens after a SARS-CoV-2 infection. They found that the combination of SARS-CoV-2 and immune cells reduced the heart’s ability to contract and pump. To understand why, the researchers turned to mitochondria, the tiny energy storehouses that power the muscle’s beating movements. They showed that SARS-CoV-2 infection led to loss of mitochondria and a release of mitochondrial DNA from the heart cells into the nutrient broth used to grow the organoids.
Working with Claudia dos Santos, a scientist and critical care doctor at Unity Health Toronto, associate professor of medicine and Pitts Research Chair in Acute Care and Emergency Medicine at U of T’s Temerty Faculty of Medicine, the researchers then asked whether the presence of freely circulating mitochondrial DNA is also seen in patients experiencing COVID-19-induced heart complications.
They analyzed blood samples from patients with and without COVID-19 and found nearly two-and-a-half times higher levels of mitochondrial DNA in patients who were COVID-19-positive. Their findings point to mitochondrial DNA levels as a powerful predictor of a person’s risk of experiencing cardiac problems after SARS-CoV-2 infection.
The team also showed that a new type of cell-based therapy called exosomes – little cargo vessels that bubble off cells – could reduce inflammation and mitochondria loss, as well as improve heart function, after SARS-CoV-2 infection, highlighting their potential to repair COVID-19-associated heart damage.
By integrating blood vessels and immune cells, Lu hopes that the innovative heart-on-a-chip model can help researchers and clinicians understand and identify treatment strategies for other infection-related heart conditions.
“The good thing about our system is that it’s readily adaptable to any kind of infectious disease,” says Lu. “The other benefit is that we don’t have to rely as much on animal models. Since we’re already using human-derived cells, the clinical translatability is much higher.”
As a next step, Radisic’s group plans to use the miniature organs to uncover why males are more likely than females to experience COVID-19-associated heart complications and to examine the cardiac issues commonly seen in people with long COVID-19.
Radisic says the motivation for this work was deeply personal. She dedicated the study to her late grandmother who died from COVID-19-induced heart failure after six weeks in the intensive care unit.
“The feeling of helplessness is rather profound when a loved one is dying,” she says. “As scientists, we can take small steps toward new cures so that other people do not meet the same fate. For me, this work meant overcoming the feeling of helplessness.”
The work was supported by investments from the Canada Foundation for Innovation and the creation of the U of T COVID-19 biobank and the Precision Medicine in Critical Care (PREDICT) Biobank at Unity Health Toronto – and by the contributions of patients and families that donated biological samples, making significant advances in research possible.