Breast cancer is very common. So much so, in fact, that it is the most commonly diagnosed type of cancer worldwide. This also means that a lot of research has already been done on breast cancer, so we know much more today than we did ten years ago, for example. Nevertheless, many people still die from this disease. In addition, many people still do not know that both men and women, young and old, can get breast cancer. All the more reason for Stacey Joosten to devote her PhD research to increasing the knowledge on breast cancer – and specifically the kind that is sensitive to the hormone estrogen. She defended her dissertation at the Department of Biomedical Engineering on March 26.
There are several types of breast cancer. The most common forms are tumors that are sensitive to the hormone estrogen. Estrogen is a hormone produced by younger women in the ovaries, for instance, but is also found in the birth control pill.
This form of breast cancer has an antenna (receptor) that responds positively to estrogen – called an estrogen receptor – so these tumors are often referred to as ‘ER+ breast cancer’ in the medical community.
Hormone receptors
“ER is a hormone receptor,” explains Stacey Joosten, newly minted doctor in Biomedical Engineering. “It’s found in all breasts and causes, for example, breast growth when estrogen is added. That’s a normal process, such as during puberty or pregnancy.”
“But in a tumor, certain cells have become ‘addicted’ to estrogen and won’t stop growing as long as estrogen is supplied. So that’s how the tumor grows and grows.”
ER+ breast cancer treatments
As a result, most treatments for this type of breast cancer target the tumor’s ‘estrogen addiction’. Patients are often given anti-hormonal treatment to inhibit the tumor. This works fine for a portion of patients. But for thirty to forty percent of patients, this treatment ceases to work after a while.
“Researchers and physicians would like to better understand how (and why) this estrogen receptor works. How does this receptor behave and what makes it sensitive or not sensitive to treatment? That’s what I’ve been diving into,” says Joosten.
“We hope that more insights will lead to smarter use of existing treatments. And perhaps new treatments can be developed based on those insights? For this reason, I researched the literature on this subject, supplemented it with new studies and compiled them in my dissertation.”
Research on the Ki-67 protein
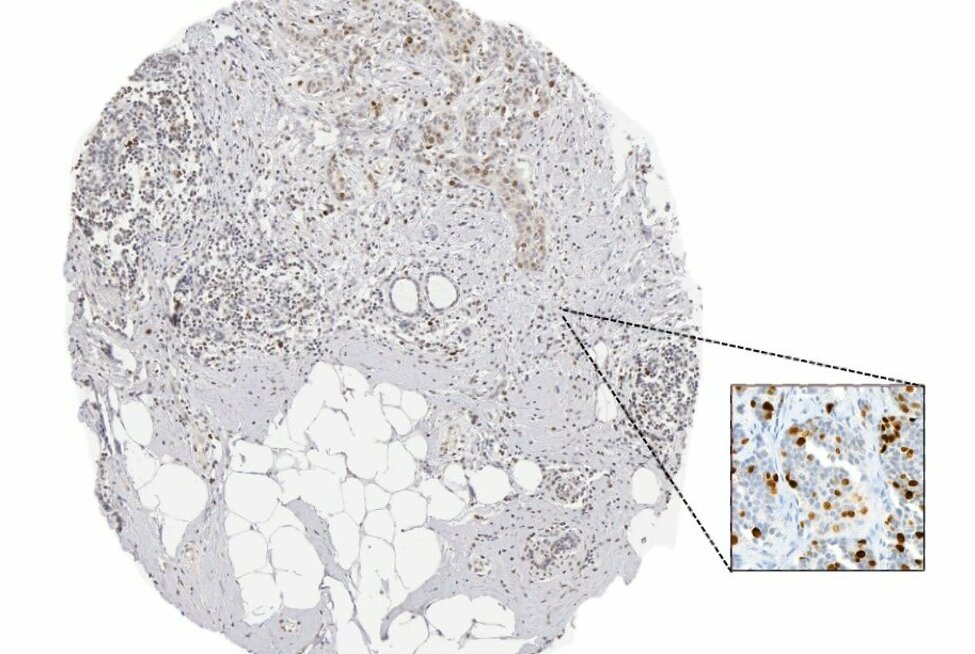
Joosten and her colleagues investigated a protein with the impressive name ‘Ki-67’. Ki-67 is a protein that indicates cell growth and is often used in the clinic and in research to determine whether anti-hormonal therapy is succeeding.
The research involved taking tumor tissue from certain patients before treatment and a few weeks after. A pathologist then assessed, under the microscope, whether the tumor had slowed down as a result of the treatment by decreasing the amount of Ki-67.
Joosten: “By staining the piece of tissue for the Ki-67 protein, the pathologist could better estimate the growth rate of the tumor. In fact, we already knew from the literature that a good predictor of the effect of the treatment is when the amount of Ki-67 decreases in postmenopausal women following treatment. And that’s also a reasonable predictor of whether the treatment will also have an effect on the tumor over a longer period of time.”
In the research, Joosten deployed several techniques, including artificial intelligence (AI), to estimate whether the Ki-67 protein is also a good predictor for breast cancer treatment in premenopausal women.
Ki-67 is used in the clinic and research on premenopausal women, but how well Ki-67 predicts response to therapy has never actually been researched for this group of patients. In addition, AI can be used to assess Ki-67 decrease much faster and more reliably than pathologists.
Tumor cells escape treatment
During her research, Joosten also uncovered more unexpected insights. For example, she examined the widely used anti-hormonal drug Tamoxifen. In some patients, Tamoxifen no longer works after years of use.
“We saw in the tumors of patients that after only a few weeks of Tamoxifen treatment, NF-κB signaling is activated. We then demonstrated in cell lines and a mouse model that activation of that NF-κB signaling allows cells to escape Tamoxifen,” says Joosten.
“In the literature, it had long been suspected that the activation of NF-κB signaling may contribute to this escape from long-term Tamoxifen treatment. But we now see for the first time that NF-κB signaling is activated even after a short treatment with Tamoxifen.”
“When we treated mice with Tamoxifen and an inhibitor of NF-κB signaling, all tumor cells were inhibited. We therefore suspected that combining Tamoxifen with an NF-κB inhibitor may have a positive effect on patients as well.”
Difference between men and women with breast cancer
Joosten also investigated whether the DNA binding of estrogen receptors works differently in men and women. In doing so, she also examined the receptors for other hormones such as testosterone and progesterone, for instance.
In breast cancer research, the gender bias is the complete opposite. After all, there are no laboratory models of male breast cancer patients.
Stacey Joosten
“In breast cancer research, the gender bias is the complete opposite. After all, there are no laboratory models of male breast cancer patients,” Joosten notes.
“That’s what makes our research so valuable. We examined pieces of tumor tissue from male breast cancer patients and were the first in the world to map the DNA binding of estrogen receptors and other hormone receptors in men. We made that research data available via open science. It’s a huge step in the right direction to a better understanding of breast cancer in men as well.”
“In general, the difference with women did not appear to be too great, but the formulas that use this DNA binding info to predict prognosis in women with breast cancer did not work for men. We therefore came up with a new formula specifically for men,” Joosten says.
The DNA binding
Finally, Joosten further explored the DNA binding of the estrogen receptor. “The estrogen receptor causes growth by binding to DNA in lots of places and triggering growth processes there. Why does the estrogen receptor stick in some places in the DNA in almost every breast cancer patient and in some places in only a few?” Joosten wondered.
Indeed, the DNA binding of estrogen receptors differed greatly between tumors. Yet from the outside, those tumors all looked like the ER+ type of breast cancer.
“There do appear to be biological differences between these tumors, which explain the differences in DNA binding or sticking. We also saw that specific sites proved to be very popular for estrogen receptors. At sites in which the estrogen receptor ‘sticks’ to the DNA in many patients, small differences in DNA between patients were found to occur more often. Those differences are associated with each person’s individual risk of estrogen-sensitive breast cancer.”
“Our research shows that such a small DNA change can cause the receptor at such a location to more or less ‘stick’ to the DNA. That can have an effect on the genes that are turned on or off by this DNA-bound ER (like a kind of switch). And that potentially influences the risk of breast cancer,” Joosten concludes.
One thing is certain: her research is helping to increase the knowledge on the treatment of breast cancer patients, whether they are men or older and younger women.